How 276/277 EDI Transactions Simplify Claim Status Tracking in Healthcare

Consider how convenient it is to track a package ordered online. You receive updates at every stage—shipped, in transit, or delivered. This level of transparency not only keeps you informed but also reduces uncertainty. In the healthcare industry, similar transparency in tracking insurance claim status is crucial, as it directly impacts revenue cycles and operational efficiency.
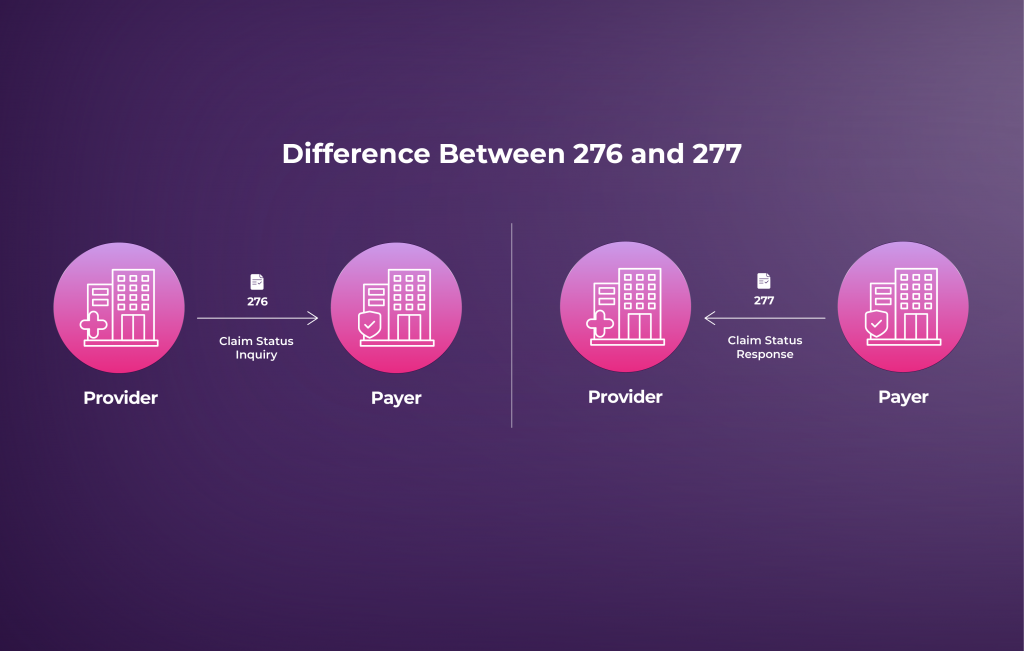
This is where 276/277 EDI transactions revolutionize the process. The 276 Claim Status Inquiry allows healthcare providers to request updates on submitted claims, while the 277 Claim Status Response provides detailed information from payers. Together, these transactions automate and streamline claim status tracking, enabling accurate and timely updates.
In this blog, we will explore how 276/277 EDI transactions simplify communication, save time, and help healthcare providers maintain financial health. Understanding these transactions is essential for operational efficiency, whether you’re dealing with denied claims or ensuring smooth reimbursements.
What Are 276/277 EDI Transactions?
The 276/277 EDI transactions are part of the ANSI X12 standards, designed to simplify communication between healthcare providers and payers. These transactions are critical in managing and tracking the status of healthcare claims.
276: Health Care Claim Status Inquiry
A 276 transaction is initiated by the healthcare provider, billing agency, or clearinghouse to inquire about the status of previously submitted healthcare claims. It includes details such as:
- Patient Information: Name, date of birth, ID numbers.
- Provider Details: NPI, contact information.
- Claim Details: Claim ID, service dates, billed amounts.
277: Health Care Claim Status Response
The 277 response provides updates on the claim’s status, indicating whether it is:
- Accepted: Under review by the payer.
- Denied: The claim was rejected with an explanation.
- Pending: Additional information is required.
- Paid: The claim has been processed, and payment has been issued.
Technical Structure of 276/277 Transactions
Both 276 and 277 transactions follow the ANSI X12 format, which includes specific segments for organizing and transmitting claim information. Key segments include:
276 Key Segments:
- ISA (Interchange Control Header): Identifies the sender and receiver.
- NM1 (Name): Details for the provider, payer, and patient.
- DTP (Date/Period): Specifies service dates.
277 Key Segments:
- STC (Status Information): The current status of the claim.
- MSG (Message Text): Explains the claim status and outlines next steps.
Simplified Workflow for 276/277 Transactions
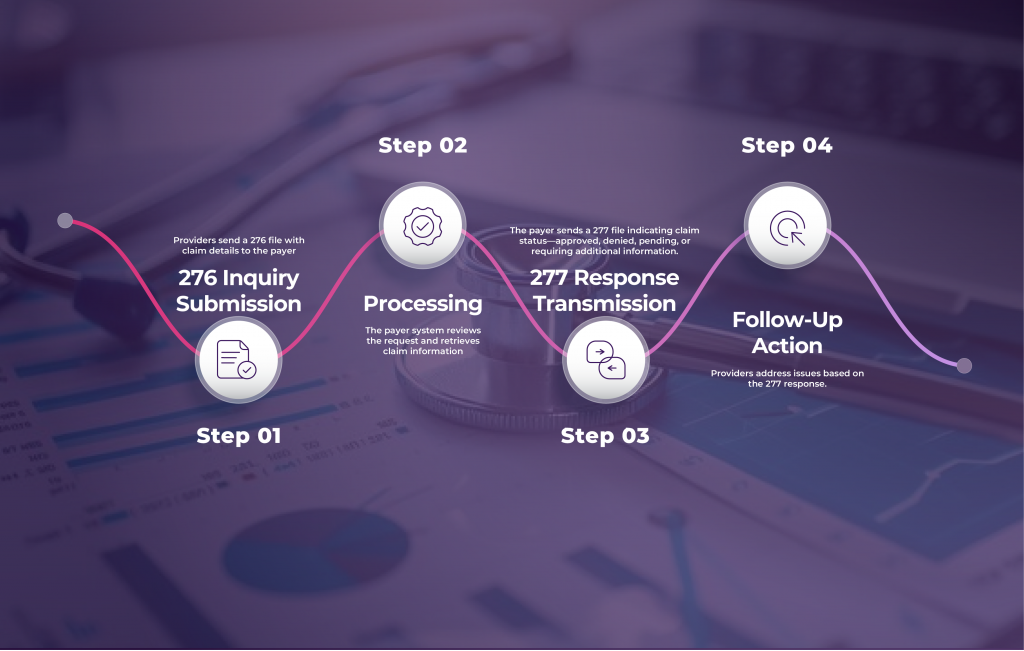
1. Claim Submission:
The provider submits a healthcare claim (via 837 transactions) to the payer, detailing patient, service, and billing information.
2. 276 Inquiry Generation:
The provider sends a 276 Claim Status Inquiry to request an update on the submitted claim.
3. Payer Receives and Processes the 276:
The payer validates the inquiry and searches for the claim in their system.
4. 277 Response Generation:
The payer generates a 277 Claim Status Response with an update on the claim’s status, such as accepted, denied, pending, or paid.
5. Provider Action:
The provider reviews the 277 response and may take corrective actions if the claim is pending or denied.
Key Benefits of 276/277 Transactions
- Efficiency: Reduces time spent on manual phone calls or emails for claim updates.
- Accuracy: Minimizes errors by providing standardized electronic communication.
- Timeliness: Offers real-time updates on claim status, enabling faster decision-making.
- Cost-Effectiveness: Automates repetitive tasks, reducing administrative costs.
Practical Examples of 276/277 EDI in Action
Batch Processing for Claims: A hospital submits batches of 276 inquiries for claims filed the previous month. The payer responds with a 277-update indicating which claims are in process, denied, or require additional documentation.
Real-Time Inquiries: A clinic uses an EDI platform to send 276 requests and receive 277 responses in real time, enabling quick resolution of denied claims.
Error Correction: Providers receive detailed denial codes in the 277 response, allowing them to quickly address issues such as incorrect diagnosis codes or missing patient details.
Simplifying Claim Status Tracking for Healthcare Providers
By leveraging 276/277 EDI transactions, healthcare providers can automate and streamline the claim status inquiry and response process. This improves transparency, reduces manual work, and enhances operational efficiency, allowing providers to focus more on patient care and less on administrative tasks.
Are you ready to simplify your healthcare claims process? Explore how Zenbridge EDI solutions can help you optimize claim status tracking and improve your revenue cycle management. Schedule your demo today to learn more!