Simplifying Healthcare Claims with the 837 EDI File
In modern healthcare, managing claims efficiently is essential. Imagine a clinic handling hundreds of insurance claims daily. Instead of relying on time-consuming paperwork or back-and-forth phone calls, providers use the 837 file—a secure, HIPAA-compliant electronic document that transforms the billing process.
The 837 file plays a vital role in healthcare claims management by electronically transmitting patient details, treatments, and costs to insurance companies. This streamlined process ensures faster, more accurate claim handling while helping patients avoid delays in coverage.
Let’s explore how EDI 837 transforms the healthcare billing process.
What is EDI 837?
The 837 file is a standardized electronic transaction used by healthcare providers to submit insurance claims, encounter data, and billing information to payers such as insurance companies or government agencies.
This HIPAA-compliant format enhances operational efficiency by reducing errors and accelerating reimbursements.
Key Uses of the 837 File
Healthcare providers rely on the 837 file to:
• Request reimbursement for medical services.
• Submit encounter data for payer analysis.
• Share billing details with payers securely and efficiently.
What does an 837 File Include?

An 837 document contains all the essential details for claim processing:
- Patient Information: Demographic details and insurance policy data.
- Diagnosis Codes: Reasons for the treatment or conditions addressed.
- Services Rendered: detailed descriptions of medical procedures.
- Billing Data: Costs associated with the treatment provided.
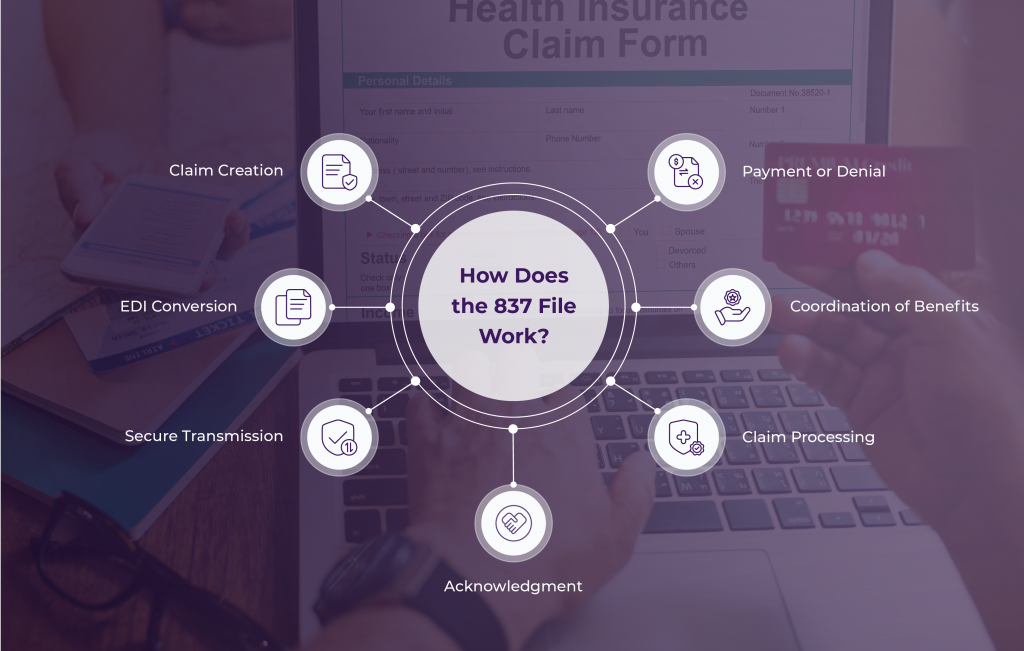
How Does the 837 File Work?
Here’s a step-by-step workflow:
1. Claim Creation: Providers compile patient and service data using billing software.
2. EDI Conversion: Data is converted into the 837 format via an EDI translator.
3. Secure Transmission: The claim is sent securely to payers using EDI VANs or direct connections.
4. Acknowledgment: Payers confirm receipt of the claim with transaction sets like 999 or 277CA.
5. Claim Processing: Payers verify and process the claim, applying coverage rules.
6. Coordination of Benefits: If the patient has multiple insurers, the system determines claim responsibilities.
7. Payment or Denial: Providers receive an 835 transaction with payment or denial details.
Benefits of EDI 837
Adopting the 837 file offers numerous advantages for providers and payers:
1. Faster Reimbursements:
Automated claims processing reduces delays.
(Example: Providers save 5 minutes per transaction on average.)
2. Improved Accuracy:
Standardization minimizes errors, reducing claim rejections.
2. Cost Savings:
Eliminating paper processes saves the Healthcare industry billions annually.
4. Compliance
Ensures adherence to HIPAA standards, safeguarding sensitive patient data.
5. Ensuring Security
EDI 837 transactions comply with HIPAA (Health Insurance Portability and Accountability Act) standards, ensuring the secure handling of sensitive patient data. Advanced encryption and access controls protect data throughout the transmission process.
Real-World Applications of the 837 File:
- Streamlined Claims Submission: Providers automate claim submissions for quicker payments.
- Error-Free Data Exchange: The standardized format reduces inaccuracies, improving claim approval rates.
- Better Patient Experience: Faster processing ensures patients avoid delays in care or unexpected out-of-pocket expenses.
Tips for Reading and Simplifying 837 Files
Understanding an 837 file is simpler with the right structure and tools:
- Segments: Data is grouped by related information, separated by tildes (~).
- Elements: Specific data points are separated by asterisks (*).
- Tools for Clarity: Software like Microsoft Word macros can organize and display 837 files in an easy-to-read format.
Why the 837 File Matters?
The 837 file is revolutionizing healthcare claims by providing a secure, efficient and accurate method for Data exchange. Its adoption reduces administrative work, ensures compliance with HIPAA standards and allows providers to focus more on delivering quality patient care.
Transform Your Claims Process with Zenbridge
Ready to simplify your healthcare claims management? Zenbridge offers HIPAA-compliant EDI solutions tailored to streamline operations, improve efficiency, and enhance accuracy.
Schedule a demo today to discover how we can revolutionize your claims process!