What is EDI 270 and EDI 271 Transaction Sets in Healthcare?
In today’s fast-paced healthcare landscape, accuracy and efficiency are essential. Verifying patient insurance eligibility is a critical process, but manual methods like paperwork and phone calls can be time-consuming and error prone. This is where Electronic Data Interchange (EDI) comes in as a game-changer.
At the heart of EDI in healthcare are the 270 and 271 transaction sets, which automate insurance eligibility and benefits verification. These standards streamline workflows, reduce errors, and improve patient care by enabling real-time communication between providers and payers.
What is EDI 270?
The EDI 270 transaction set is a standardized format used to send inquiries about a patient’s healthcare eligibility and benefit details.
Key Purposes of EDI 270:
- To verify if a patient’s insurance policy is active.
- To check coverage for specific medical services, treatments, or procedures.
For example, a healthcare provider might use EDI 270 to confirm whether a patient’s insurance covers a scheduled surgery.
What is EDI 271?
The EDI 271 transaction set is the response to an EDI 270 inquiry. It provides detailed information about the patient’s eligibility, coverage, and benefit specifics.
Key Purposes of EDI 271:
- To confirm insurance coverage status.
- To provide details like co-pays, deductibles, policy limitations, and coverage dates.
For example, after receiving an EDI 270 request, an insurer uses EDI 271 to share precise information about the patient’s benefits.
How EDI 270 and 271 Work Together
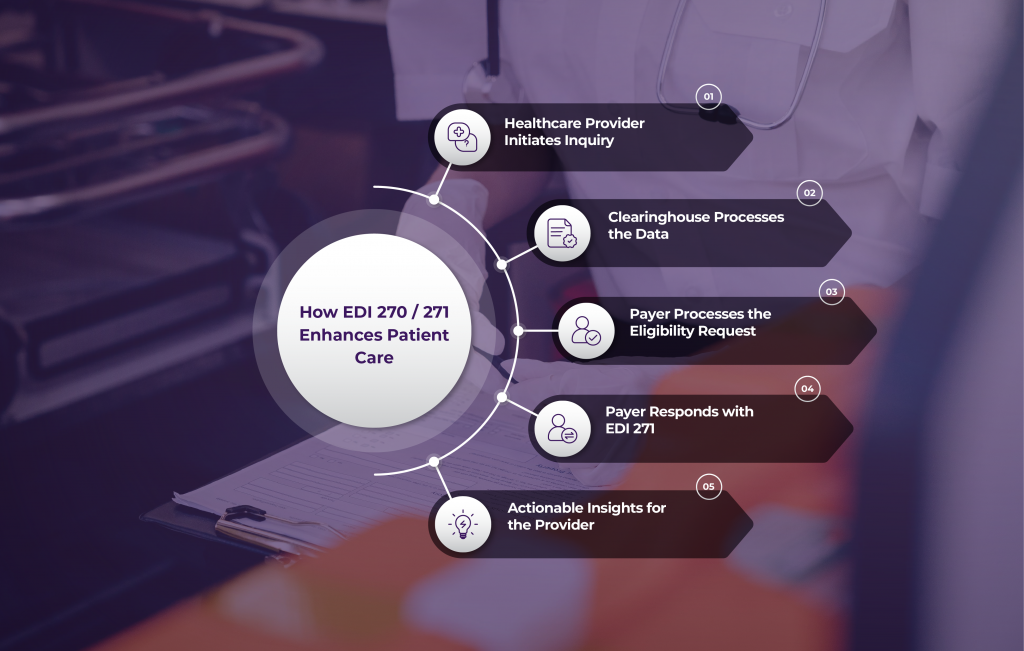
Here’s how the process flows:
- Provider Sends an Inquiry (EDI 270): A provider submits an electronic request to verify a patient’s eligibility through their EHR system.
- Clearinghouse Processes the Request: The clearinghouse ensures data is formatted correctly and securely forwards it to the payer.
- Payer Verifies Eligibility: The insurance company processes the request, checking details like policy validity and co-pay amounts.
- Payer Responds (EDI 271): The payer sends an EDI 271 response back to the provider with detailed coverage information.
- Provider Takes Action: Providers can now make informed decisions, such as proceeding with treatment, adjusting plans, or discussing payment options with the patient.
Benefits of Using EDI 270 and 271
These transaction sets bring numerous advantages to healthcare operations:
- Faster Insurance Verification: Real-time responses reduce delays.
- Reduced Claim Rejections: Minimized errors ensure accurate billing.
- Improved Patient Experience: Streamlined check-ins and billing create a smoother process.
- Compliance with HIPAA: Ensures secure and compliant data exchange.
Common Challenges and How to Overcome Them
While implementing EDI 270 and 271 is transformative, challenges exist:
- Technical Barriers
- Integrating with older systems can be tricky.
- Data formatting inconsistencies may arise.
- Solution: Work with an experienced EDI provider like Zenbridge to simplify integration and maintain compliance.
- Data Accuracy
- Outdated or incorrect patient data can lead to errors.
- Solution: Regularly validate and update data to ensure accuracy.
- Cost and Resource Constraints
- Initial setup and maintenance can be costly.
- Solution: Use scalable EDI solutions to minimize costs over time.
Key Data Elements in EDI 270 and 271
EDI 270 (Eligibility Inquiry)
- Sender and Receiver Info: Provider and insurance company details.
- Patient Info: Name, date of birth, and insurance ID.
- Service Details: Type of service requested (e.g., surgery, check-up).
EDI 271 (Eligibility Response)
- Coverage Status: Is the patient covered?
- Benefit Details: Co-pays, deductibles, and policy limits.
- Patient Responsibility: What the patient needs to pay.
Why Choose Zenbridge for EDI Solutions?
By adopting EDI 270 and 271, healthcare providers can transform their operations, reduce administrative burdens, and enhance patient care.
Zenbridge offers:
- HIPAA-compliant EDI solutions tailored to your needs.
- Seamless implementation and expert support.
- Scalable solutions that grow with your business.
Ready to optimize your insurance verification process? Visit Zenbridge.io today to schedule a demo and revolutionize your healthcare operations!